Ethionamide
Ethionamide — Description will be added later. Active ingredient: .
Select dosage
| Package | Details | Price | Savings | |
|---|---|---|---|---|
| Ethionamide 250mg 30 pill |
30 pills $ 6.00 per pill |
$ 215.99$ 179.99 | save: €36.00 | Add to Cart |
| Ethionamide 250mg 60 pill |
60 pills $ 5.62 per pill |
$ 404.39$ 336.99 | save: €67.40 | Add to Cart |
| Ethionamide 250mg 90 pill |
90 pills $ 5.24 per pill |
$ 566.39$ 471.99 | save: €94.40 | Add to Cart |
| Ethionamide 250mg 120 pill |
120 pills $ 4.77 per pill |
$ 686.39$ 571.99 | save: €114.40 | Add to Cart |
| Ethionamide 250mg 180 pill |
180 pills $ 4.31 per pill |
$ 931.19$ 775.99 | save: €155.20 | Add to Cart |
Product Information
Mastering Multidrug-Resistant Tuberculosis: Why Ethionamide is Your Essential Ally in Treatment
Tuberculosis (TB) remains a significant global health challenge, but the emergence of drug-resistant strains presents an even graver threat. When standard first-line treatments fail, clinicians and patients must turn to highly specialized, powerful agents. This article provides an in-depth, informative overview of Ethionamide, an indispensable antibiotic in the fight against resistant forms of this persistent infection. If you are searching for effective treatment for drug-resistant TB, understanding the role of this crucial medication is paramount.
Problem Description: The Rising Tide of Drug Resistance
Tuberculosis, caused by Mycobacterium tuberculosis, is typically managed with a combination of antibiotics over many months. However, non-adherence to treatment regimens, inadequate initial therapy, or the intrinsic resistance profile of certain bacterial strains leads to the development of drug-resistant TB (DR-TB). Multidrug-resistant tuberculosis (MDR-TB), resistant to at least isoniazid and rifampicin—the two most potent first-line drugs—requires second-line agents that are often less effective, more toxic, and require significantly longer treatment durations. Patients often ask, what is the best medication for MDR-TB, and the answer frequently points towards agents like Ethionamide.
The treatment landscape for MDR-TB is complex, involving regimens tailored to the specific resistance profile of the patient's infection. Traditional injectable agents, which were historically mainstays, are being phased out due to severe side effects, leading to a greater reliance on oral agents, even those with challenging side effect profiles. The urgency to find effective, tolerable oral alternatives drives much of the current research in infectious disease. Understanding the spectrum of activity is key; while some broad-spectrum antibiotics like Amoxicillin or Erythromycin are cornerstones for other infections, they lack efficacy against mycobacteria, making specialized drugs necessary.
How the Medication Helps: The Mechanism of Action of Ethionamide
Ethionamide belongs to the thioamide class of antibiotics, closely related structurally to isoniazid but possessing a distinct mechanism of action, which is crucial for overcoming resistance. It functions as a prodrug, meaning it must be metabolically activated within the Mycobacterium tuberculosis cell to become effective. This activation process, primarily mediated by the enzyme EthA (a catalase-peroxidase), converts Ethionamide into its active form, thioamide-2-oxide.
This active metabolite interferes with the biosynthesis of mycolic acids, which are essential, long-chain fatty acids that form the distinctive, waxy outer layer of the mycobacterial cell wall. Disrupting mycolic acid synthesis compromises the integrity of the cell wall, leading to cell death. Because its target pathway is different from many other antibiotics, Ethionamide is often effective even when resistance to other drugs has developed. This unique mechanism makes it a vital component in combination therapy, especially when treating complex cases like those involving resistance to fluoroquinolones, such as Ciprofloxacin or Levaquin. Many patients inquire about Ethionamide mechanism of action to better understand its necessity in their regimen.
Benefits: Why Ethionamide is Essential in Modern TB Care
The primary benefit of Ethionamide lies in its indispensable role in treating MDR-TB. As a Group A drug in WHO guidelines for the treatment of drug-resistant TB, its inclusion significantly increases the chances of achieving a microbiological cure. Its oral bioavailability is generally good, allowing for convenient administration compared to older injectable agents.
Furthermore, Ethionamide exhibits potent in vitro activity against M. tuberculosis. When used in a correctly formulated combination regimen—typically involving three or more active agents—it contributes synergistically to the overall bactericidal effect. Successful treatment of MDR-TB hinges on using multiple drugs with different mechanisms to prevent the emergence of further resistance during therapy. For patients facing lengthy, debilitating treatment courses, optimizing every drug choice is critical; those searching for where to buy Ethionamide online are often doing so under the direct instruction of their infectious disease specialist, recognizing its proven utility.
Another subtle but important advantage is its activity profile against certain non-tuberculous mycobacteria (NTM), although it is primarily known for its TB efficacy. In situations where clinicians might consider alternatives like Doxycycline or Norfloxacin for other infections, the specialized nature of Ethionamide ensures maximum targeted impact against Mycobacterium tuberculosis. Its inclusion helps shorten the duration of treatment compared to regimens relying solely on less potent second-line drugs. We are seeing growing interest in Ethionamide cost among patients seeking affordable access to this life-saving therapy.
Safety and Side Effects: Managing the Therapeutic Challenge
While highly effective, Ethionamide is notorious for its adverse effect profile, which is the main limiting factor in its use and adherence. The most common and dose-limiting side effect is gastrointestinal intolerance, including severe nausea, vomiting, dyspepsia, and abdominal pain. Another significant concern is neurotoxicity, manifesting as peripheral neuropathy, depression, drowsiness, and potential psychotic reactions in susceptible individuals. Patients must be closely monitored, especially concerning mental health status throughout treatment.
Thyroid dysfunction is another recognized side effect; hypothyroidism can occur, necessitating regular thyroid function testing (TFTs) during the treatment course. Pyridoxine (Vitamin B6) supplementation is often co-administered, similar to its use with isoniazid, to mitigate the risk of peripheral neuropathy, although this specific risk is sometimes considered lower with Ethionamide than with isoniazid, depending on the dose. It is important to compare potential side effects when considering alternatives; for instance, while antibiotics like Augmentin or Keflex generally have better GI tolerance profiles, they are ineffective against TB.
Dosage adjustments are frequently necessary to balance efficacy and tolerability. Clinicians often start treatment at a lower dose and titrate upwards slowly to help the patient acclimatize to the medication. Physicians must carefully weigh the risks of side effects against the certainty of death or severe morbidity from untreated MDR-TB. Researching Ethionamide side effects management is a standard pre-treatment step for informed patients.
Dosage and Available Forms
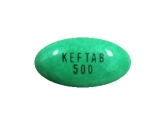
Ethionamide is typically classified as a second-line agent, and its dosing is highly individualized based on the patient's weight, renal and hepatic function, and, critically, their tolerance to the drug. The standard recommended daily dosage for adults ranges generally from 500 mg to 1000 mg, usually divided into two or three doses per day to minimize peak plasma concentrations and associated side effects. The availability of specific strengths is vital for accurate dosing. Ethionamide is most commonly supplied in tablet form, with the primary available dosage being 250 mg.
For a patient requiring 750 mg per day, this would translate to three 250 mg tablets taken throughout the day. Adherence to the prescribed schedule is non-negotiable for successful treatment of mycobacterial infections. Unlike some short-course antibiotic treatments, MDR-TB therapy utilizing Ethionamide often spans 18 to 24 months or longer, underscoring the need for robust adherence support. Patients often search for the Ethionamide 250mg tablet uses to confirm its application in their specific regimen.
If a patient is unable to tolerate the full dose due to severe nausea, the physician may reduce the dose, although this must be balanced against the risk of treatment failure. In cases where an alternative second-line agent is being considered, providers often review therapies like those involving Cleocin (Clindamycin) or Omnicef (Cefdinir) for other infections, but these are not direct substitutes for the antimycobacterial action of Ethionamide. It is essential that patients confirm their prescription details, including the exact required dosage, with their pharmacy, specifically noting the Ethionamide Dosages: 250mg availability.
Reviews/Social Proof: Patient Experiences with Ethionamide
Patient testimonials regarding Ethionamide are often polarized, largely reflecting the severity of the side effects versus the relief of having an effective drug against a life-threatening disease. Many patients report significant initial GI upset, describing it as an unavoidable hurdle. However, the overwhelming sentiment among survivors of MDR-TB is gratitude for the drug’s efficacy. Stories often highlight that while the journey was tough, overcoming the side effects was manageable with physician support, dietary adjustments, and anti-nausea medication.
One common theme in patient forums is the success stories shared after completing the long treatment course, emphasizing that the temporary discomfort of Ethionamide was a small price to pay for beating MDR-TB. A patient success story might read: "I dreaded taking Ethionamide every day, but three years later, my chest X-rays are clear. It’s a tough drug, but it worked where others failed." This type of anecdotal evidence underscores the high stakes involved. In contrast, when patients research less intense antibiotics for minor ailments, they might see positive reviews for drugs like Duricef, but these comparisons are irrelevant when facing MDR-TB.
Furthermore, healthcare providers frequently discuss the necessity of Ethionamide in their published clinical notes. The consensus among infectious disease specialists supports its continued use as a core component in almost all MDR-TB regimens. When individuals search for patient reviews of Ethionamide, they are seeking validation that this difficult treatment path leads to a positive outcome, which, statistically, it often does when adherence is maintained.
Price and Where to Buy: Ensuring Access to Essential Antibiotics
As a crucial drug for a severe, often neglected disease, the accessibility and cost of Ethionamide can be a significant concern, particularly in resource-limited settings. Pricing structures for second-line TB drugs vary dramatically depending on the supplier, regulatory environment, and volume purchased. While some countries benefit from global procurement mechanisms that subsidize costs, individual patients often face higher out-of-pocket expenses, leading to searches for discounted Ethionamide.
It is imperative that patients purchase Ethionamide only through licensed, reputable pharmacies or healthcare systems. Self-medication or purchasing from unregulated sources poses extreme risks, not only due to counterfeit products but also because therapeutic drug monitoring is essential for this medication. Reliable sources ensure the Ethionamide Category: Antibiotics classification and quality standards are met.
For international patients or those facing high local costs, exploring established online pharmacies that specialize in prescription medications under physician oversight is an option, provided they adhere to all legal requirements for dispensing prescription-only drugs. If you are looking for alternatives for general bacterial infections, you might look up Tobramycin and dexamethasone, but for TB, Ethionamide remains critical. We strongly advise consulting your healthcare provider to navigate the procurement process safely and affordably. Many patients also investigate Ethionamide purchase options to secure long-term supplies.
Frequently Asked Questions (FAQ) about Ethionamide
Q1: Can Ethionamide be taken alone for TB?
A1: Absolutely not. Ethionamide, like all anti-TB agents, must be administered as part of a combination regimen involving at least two, and preferably three or more, other active anti-TB drugs. Using it as monotherapy virtually guarantees the rapid selection and proliferation of resistant strains, leading to XDR-TB (Extensively Drug-Resistant TB).
Q2: How long do I need to take Ethionamide?
A2: The duration of therapy involving Ethionamide is typically dictated by the overall MDR-TB treatment protocol, which usually mandates treatment continuation for at least 18 to 24 months after achieving culture conversion (when sputum tests no longer show active bacteria). This is a significant time commitment.
Q3: What should I do if I miss a dose of Ethionamide?
A3: Missing doses is extremely dangerous in TB treatment. If you realize you missed a dose shortly after the scheduled time, take it, unless it is almost time for the next dose. Never double up on doses. Immediately contact your healthcare provider or TB clinic to discuss missed doses, as they may require adjustments to prevent resistance development. Patients often ask what happens if I miss Ethionamide dose.
Q4: Is there a difference between Ethionamide and Prothionamide?
A4: Prothionamide is the S-enantiomer of Ethionamide (the racemic mixture). While Prothionamide is generally considered more potent and may have a slightly different side effect profile, Ethionamide (250mg tablets) remains the more widely available and utilized formulation globally for MDR-TB treatment protocols.
Q5: Can I stop taking Ethionamide once I start feeling better?
A5: No. Feeling better only indicates that the drug burden has suppressed the bacteria significantly. Stopping early, even if symptoms disappear, leaves behind dormant or partially susceptible bacteria that can reactivate the disease, often in a more resistant form. Continuing the full prescribed course, including Ethionamide, is essential for cure.
Conclusion — Reclaiming Your Health with Precision Medicine
Ethionamide, available in its 250mg dosage, stands as a cornerstone therapy in the challenging fight against multidrug-resistant tuberculosis. While its profile necessitates careful management of potential side effects like GI distress and neurological symptoms, its proven efficacy in combination regimens cannot be overstated. It offers a vital pathway to cure when first-line drugs fail, acting through its unique inhibition of mycolic acid synthesis. If you or a loved one has been diagnosed with MDR-TB, embrace the prescribed regimen, including this powerful antibiotic. Trust in the established protocols that utilize this essential tool.
Do not delay starting or continuing your vital treatment. Speak with your infectious disease specialist today about ensuring you have consistent access to high-quality Ethionamide 250mg tablets to complete your journey toward a TB-free future.
Take Control of Your Treatment: Consult Your Physician Immediately to Secure Your Prescription for Ethionamide Today.
Why buy here?
- Discreet packaging
- Pharmacist support
- Money-back guarantee